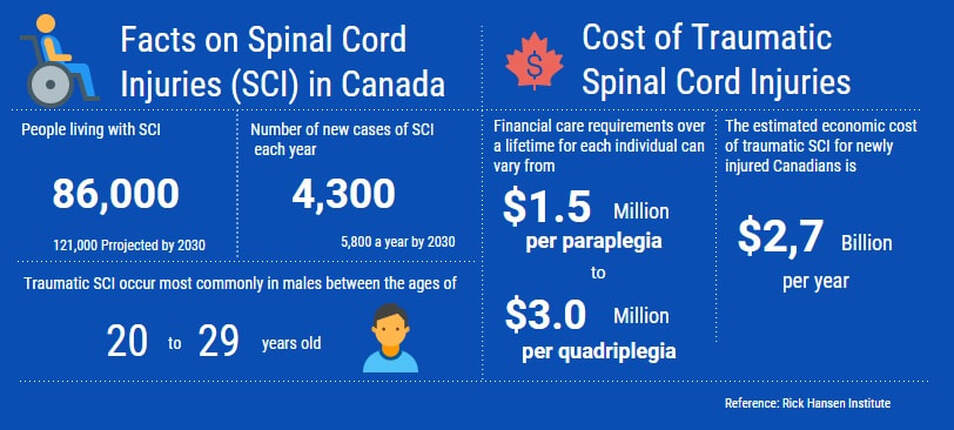
Spinal Cord Injuries at a Glance
What is a Spinal Cord Injury?
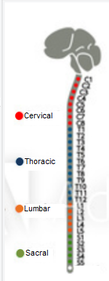
The spinal cord is a bundle of nerves that carries sensory, motor and reflex signals between the brain and the body. It is surrounded by rings of bone called vertebrae, which are divided into segments. Injury to the spinal cord may interfere with the nerve conduction leading to sensory and motor impairments. The higher the injury on the spinal cord, the more dysfunction can occur.
Spinal cord injuries can be divided into two types of injury :
The level of paralysis is determined by where the damage occurs in the neck or back.
Spinal cord injuries can be divided into two types of injury :
- Complete injury means that there is no function below the level of the injury - either sensation and movement. Complete injuries can occur at any level of the spinal cord.
- Incomplete Spinal Cord Injury: An incomplete injury means there is some function below the primary level of injury. A person with an incomplete injury may be able to move one limb more than another, may be able to feel parts of the body that cannot be moved. Incomplete injuries can occur at any level of the spinal cord.
The level of paralysis is determined by where the damage occurs in the neck or back.
- Paraplegia: It typically affects the trunk and both legs, but not the arms. This is usually a result of injuries at the thoracic and lumbar levels.
- Quadriplegia or Tetraplegia: It results from injury to the spinal cord in the neck (cervical level) and is associated with total or partial loss of function in the legs, arms and trunk (from the neck down).
Impacts of the Spinal Cord Injuries
Spinal cord injuries (SCI) have a devastating impact on the health and well being of individuals. Many would categorize SCI as one of the greatest survivable catastrophes experienced by a human being.
As a result, individuals with a spinal cord injury may not be able to perform activities in a way that is otherwise considered normal for them. This activity limitation challenges the individual’s participation in day-to-day life situations and activities.
There is a great risk that they will develop a pressure ulcer, fracture or heart disease, among other health issues.
Research has shown that denervation of the muscles below the level of the spinal cord lesion causes gradual deconditioning of the muscle resulting in structural changes such as decrease in muscle mass and number of muscle fibres (Biering-Sorensen et al., 2009). Also, another research indicates that there is a transformation from slow twitch fatigue resistant muscle fibers to fast twitch, fast fatiguing fibres. These physiological changes not only affect the functional capacity of the muscles, but also the metabolic functions of the muscles leading to metabolic disorders such as obesity, dyslipidemia and diabetes (Manns et al., 2005).
Another physical impact is that the bone mass below the level of lesion decreases rapidly after the first few years of injury and then continues to decrease gradually, unless addressed from the time of injury. Unloading is an important factor for osteoporosis along with neuronal and hormonal changes after a spinal cord injury (Jiang et al., 2006).
As a result, individuals with a spinal cord injury may not be able to perform activities in a way that is otherwise considered normal for them. This activity limitation challenges the individual’s participation in day-to-day life situations and activities.
There is a great risk that they will develop a pressure ulcer, fracture or heart disease, among other health issues.
Research has shown that denervation of the muscles below the level of the spinal cord lesion causes gradual deconditioning of the muscle resulting in structural changes such as decrease in muscle mass and number of muscle fibres (Biering-Sorensen et al., 2009). Also, another research indicates that there is a transformation from slow twitch fatigue resistant muscle fibers to fast twitch, fast fatiguing fibres. These physiological changes not only affect the functional capacity of the muscles, but also the metabolic functions of the muscles leading to metabolic disorders such as obesity, dyslipidemia and diabetes (Manns et al., 2005).
Another physical impact is that the bone mass below the level of lesion decreases rapidly after the first few years of injury and then continues to decrease gradually, unless addressed from the time of injury. Unloading is an important factor for osteoporosis along with neuronal and hormonal changes after a spinal cord injury (Jiang et al., 2006).
Exercise-based Intensive Program Approach
Traditionally, compensatory approach not only limits individuals with spinal cord injury to use residual function in the affected areas but also further weakens the affected areas below the level of the spinal cord lesion. The belief that the nervous system is hard wired and irreparable has left clinicians and therapists with the option of training spinal cord injuries to accommodate existing impairments and use assistive devices such as orthotics and wheelchairs to improve participation in day-to-day life situations and activities.
In recent years, there has been a shift in the way the concept of physical rehabilitation is viewed. Researchers have categorically stated that the field of modern neurorehabilitation no longer aims at compensation for disabilities; rather, it works through a spectrum of therapeutic interventions to gain functional recovery by use of “restorative neurology,” the practice of facilitating neural plasticity (Tansey, 2010).
Physical activity is one such essential therapeutic intervention. Researchers have provided preliminary evidence to show that the nervous system is not hard-wired but malleable, and that function lost due to a spinal cord injury can be recovered. The evidence is particularly strong for walking recovery post spinal cord injury.
The ultimate aim of any physical rehabilitation program for a spinal cord injury should be to improve quality of life by improving function below the level of injury in each individual.
In recent years, there has been a shift in the way the concept of physical rehabilitation is viewed. Researchers have categorically stated that the field of modern neurorehabilitation no longer aims at compensation for disabilities; rather, it works through a spectrum of therapeutic interventions to gain functional recovery by use of “restorative neurology,” the practice of facilitating neural plasticity (Tansey, 2010).
Physical activity is one such essential therapeutic intervention. Researchers have provided preliminary evidence to show that the nervous system is not hard-wired but malleable, and that function lost due to a spinal cord injury can be recovered. The evidence is particularly strong for walking recovery post spinal cord injury.
The ultimate aim of any physical rehabilitation program for a spinal cord injury should be to improve quality of life by improving function below the level of injury in each individual.